Massage for Back Pain: Does It Really Work? Expert Guide
Evidence-based insights on how massage therapy can help relieve your back pain

If you're reading this, chances are your back hurts. You're not alone—back pain is one of the most common reasons people seek medical care, affecting approximately 80% of adults at some point in their lives. It's also one of the leading causes of missed work and disability worldwide. So when someone suggests massage therapy, you might wonder: does it actually help, or is it just a temporary feel-good treatment?
The short answer is yes—massage therapy can be genuinely effective for many types of back pain. But the complete answer is more nuanced. The effectiveness depends on what's causing your pain, which type of massage you receive, and how it fits into your overall treatment approach. Let's examine the evidence and help you understand whether massage might work for your specific situation.
What the Research Says About Massage for Back Pain
The scientific evidence supporting massage therapy for back pain has grown substantially over the past two decades. Multiple systematic reviews and clinical trials have examined massage therapy's effectiveness, and the results are largely positive—with some important caveats.
Key Research Findings
A landmark study published in the Annals of Internal Medicine found that massage therapy provided significant relief for chronic lower back pain. Participants who received weekly massages for 10 weeks showed greater improvement in function and pain reduction compared to those receiving usual care. Remarkably, benefits persisted for at least 6 months after treatment ended.
The Cochrane Collaboration, known for rigorous evidence reviews, concluded that massage therapy may be beneficial for patients with subacute and chronic nonspecific low back pain, particularly when combined with exercises and education. They noted that massage appears most effective when given alongside other active treatments.
What Type of Back Pain Responds Best?
Research indicates massage is most effective for:
- Nonspecific low back pain (pain without a clear structural cause)
- Muscle tension and muscle spasm-related pain
- Subacute back pain (lasting 4-12 weeks)
- Chronic back pain as part of a multimodal treatment approach
- Back pain associated with stress and anxiety
- Post-exercise muscle soreness in the back
Evidence is less conclusive for acute back pain (less than 4 weeks) and structural issues like herniated discs, though many patients report symptomatic relief even in these cases. The key is understanding that massage addresses certain aspects of back pain—muscle tension, circulation, nervous system regulation—rather than fixing underlying structural problems.
How Massage Helps Back Pain: The Mechanisms
Understanding how massage works helps explain why it's effective for some types of back pain and not others. Multiple physiological mechanisms contribute to pain relief:
1. Muscle Relaxation
Tight, contracted muscles are a major source of back pain. When muscles stay tense—whether from poor posture, overuse, or protective guarding around an injury—they become painful and can compress nerves. Massage directly addresses this by mechanically relaxing muscle fibers, releasing contracted tissues, and reducing muscle spasm—the often the most immediately noticeable benefit: you can feel muscles 'letting go' during treatment.
2. Improved Circulation
Massage increases blood flow to treated areas, bringing oxygen and nutrients while removing metabolic waste products that accumulate in tense muscles. Lactic acid and other byproducts of muscle metabolism can contribute to pain and stiffness; enhanced circulation helps clear these substances. The warming effect of increased blood flow also helps relax tight tissues.
3. Pain Gate Mechanism
Your nervous system can only process so much sensory information at once. The pressure and touch sensations from massage compete with pain signals for attention, effectively 'closing the gate' on pain transmission to your brain. This explains why rubbing a sore spot provides immediate—if temporary—relief. Therapeutic massage extends and amplifies this effect.
4. Endorphin Release
Massage stimulates the release of endorphins—your body's natural painkillers. These neurotransmitters bind to opioid receptors in your brain and spinal cord, reducing pain perception and creating feelings of wellbeing. Research shows that even a single massage session can increase endorphin levels.
5. Reduced Cortisol and Stress Response
Chronic pain and stress create a vicious cycle—pain causes stress, and stress amplifies pain perception. Massage has been shown to reduce cortisol (the stress hormone) while increasing serotonin and dopamine. This neurochemical shift helps break the pain-stress cycle and can reduce both the physical and emotional components of chronic back pain.
6. Fascial Release
Fascia—the connective tissue that surrounds muscles and organs—can become restricted and contribute to back pain. Massage techniques, particularly myofascial release, help restore mobility to fascial tissues. This is especially relevant for chronic back pain, where fascial restrictions often develop over time.
Best Types of Massage for Back Pain
Not all massages are created equal when it comes to treating back pain—different techniques offer different benefits, and the best choice depends on your specific condition:
| Massage Type | Best For | Intensity | How It Helps |
|---|---|---|---|
| Deep Tissue | Chronic muscle tension, knots | Firm to intense | Releases deep muscle restrictions, breaks adhesions |
| Swedish | General back pain, relaxation | Light to moderate | Improves circulation, reduces overall tension |
| Trigger Point | Referred pain, specific tight spots | Moderate to firm | Deactivates pain-triggering muscle knots |
| Myofascial Release | Chronic pain, restricted movement | Light to moderate | Releases fascial restrictions, improves mobility |
| Thai Massage | Stiffness, limited flexibility | Moderate | Combines stretching with compression |
| Sports Massage | Activity-related back pain | Varies | Addresses exercise-induced tension and strain |
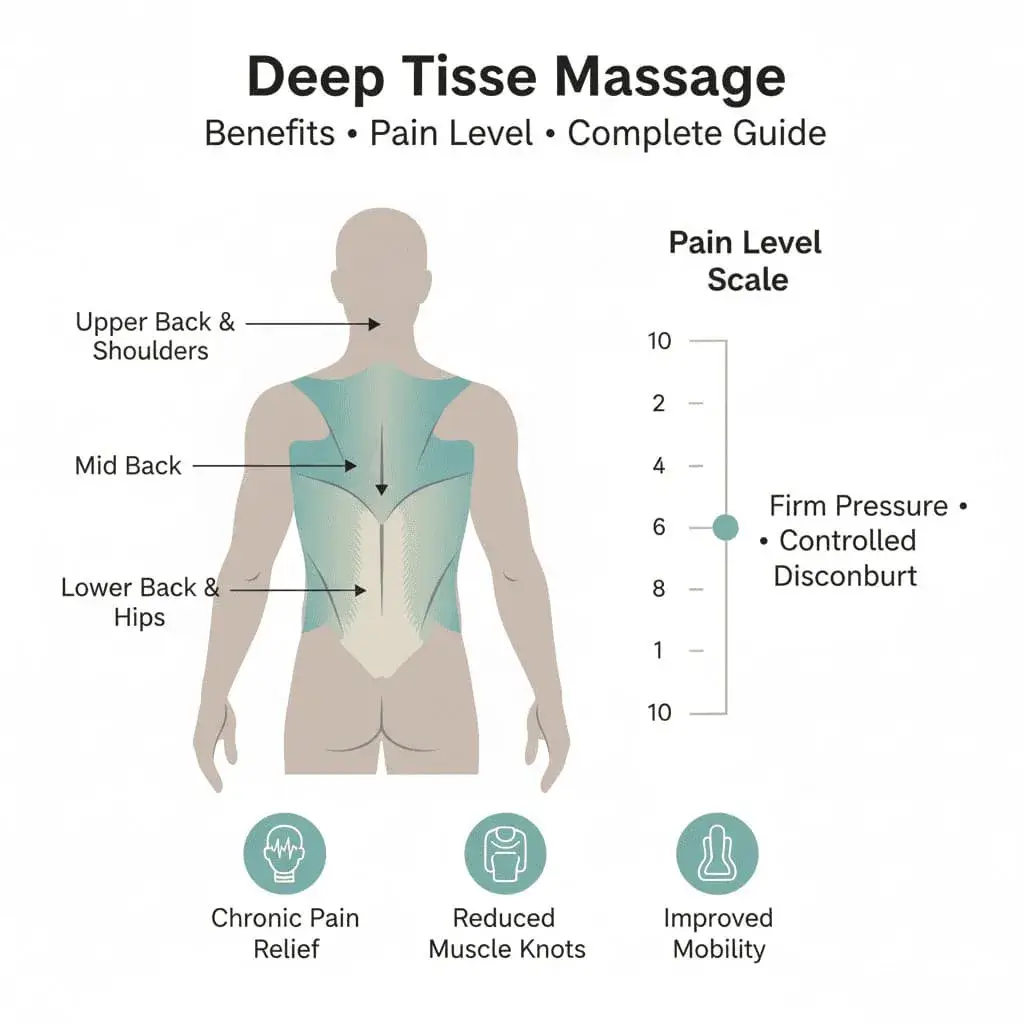
Deep Tissue Massage for Back Pain
Deep tissue massage uses slow, firm strokes to reach deeper layers of muscle and fascia. It's particularly effective for chronic back pain because it can access muscles that superficial techniques don't reach—like the quadratus lumborum and erector spinae that often contribute to lower back pain. The intense pressure breaks up adhesions (bands of rigid tissue) and releases chronic muscle tension.
Deep tissue work can be uncomfortable during treatment, but many people find it provides more lasting relief than gentler approaches. Communication with your therapist about pressure is essential—effective deep tissue work finds the edge between therapeutic discomfort and actual pain.
Trigger Point Therapy
Trigger points are hyperirritable spots in muscles that cause local and referred pain. A trigger point in your upper back might cause pain that radiates to your shoulder; one in your gluteal muscles might send pain down your leg (often confused with sciatica). Trigger point therapy applies sustained pressure to these spots until they release, which can dramatically reduce pain in seemingly unrelated areas.
If your back pain includes specific tender points that refer pain elsewhere when pressed, trigger point therapy may be particularly effective. Many chronic back pain sufferers have multiple active trigger points that perpetuate their pain cycle.
Swedish Massage
Don't underestimate Swedish massage for back pain—while it's often considered a 'relaxation' massage, research shows it can be just as effective as structural techniques for chronic low back pain. The flowing strokes improve circulation, reduce overall muscle tension, and activate your parasympathetic nervous system—helping your body shift from 'fight or flight' to 'rest and heal' mode.
Swedish massage is often a good starting point if you're new to massage therapy or if your back is too sensitive for deep tissue work. It's also valuable for back pain that's strongly connected to stress and anxiety.
Massage for Different Types of Back Pain
Lower Back Pain
Lower back pain is the most common type, and fortunately, it often responds well to massage therapy. The lumbar region is supported by multiple muscle groups that can become tight and painful—including the erector spinae, quadratus lumborum, psoas, and gluteal muscles. A skilled massage therapist will address not just your lower back, but also your hips, glutes, and even your upper legs, since these areas directly affect lumbar function.
For chronic lower back pain, a combination of deep tissue work on specific tight muscles and broader relaxation techniques often works best. Regular sessions (weekly to bi-weekly) initially, transitioning to monthly maintenance, can help manage ongoing issues.
Upper Back and Shoulder Pain
Upper back pain often stems from poor posture, particularly the forward-head position common in desk workers. The muscles between your shoulder blades (rhomboids, middle trapezius) become overstretched and painful, while chest muscles tighten. Massage therapy for upper back pain typically focuses on releasing the tight chest muscles while addressing trigger points in the upper back and neck.
This type of pain often requires work beyond just the painful area—treating the neck, shoulders, and chest muscles that contribute to postural dysfunction. Many therapists incorporate stretching and movement education alongside massage.
Sciatica and Radiating Pain
Sciatica—pain that radiates from your lower back down your leg—can have multiple causes, not all of which massage can address. If your sciatica is caused by a herniated disc pressing on a nerve root, massage won't fix the disc problem. However, it can provide significant relief by relaxing the muscles that spasm around the irritated nerve and may be compressing it further.
Piriformis syndrome—where the piriformis muscle in your buttock compresses the sciatic nerve—responds particularly well to massage. Releasing this deep hip rotator can dramatically reduce sciatic symptoms. If you have sciatica, work with both a healthcare provider (to identify the cause) and a massage therapist (to address muscular components).
What to Expect from Massage Treatment
During Your First Session
Your massage therapist will begin with an assessment—asking about your pain history, location, intensity, what makes it better or worse, and any relevant medical conditions. Be specific: 'My lower back aches after sitting for more than an hour' is more helpful than 'my back hurts.' This information guides treatment.
You'll typically lie face-down on a massage table, though positioning may be adjusted based on your comfort and the areas being treated. For back pain, expect significant attention to your back, but also work on related areas—your glutes, hips, and possibly legs for lower back pain, or your neck and shoulders for upper back issues.
Realistic Expectations
After a single session, you'll likely feel some immediate relief—reduced tension, improved mobility, and often a general sense of relaxation. However, one massage rarely resolves chronic back pain. Think of massage as cumulative: each session builds on the last. Research suggests a series of treatments (often 6-10 sessions) provides the best outcomes for chronic conditions.
Some people experience temporary soreness after deep tissue work—similar to post-exercise muscle soreness. This typically resolves within 24-48 hours and doesn't indicate harm. Staying hydrated and gentle movement can help.
| Timeframe | What to Expect | Notes |
|---|---|---|
| Immediately after | Reduced tension, relaxation, temporary relief | Effects may last hours to days |
| After 2-3 sessions | Noticeable pain reduction, improved mobility | Cumulative benefits begin building |
| After 6-10 sessions | Significant improvement for many chronic conditions | Research-supported treatment duration |
| Ongoing maintenance | Sustained benefits, prevention of recurrence | Monthly sessions often sufficient |
Maximizing Massage Benefits for Back Pain
Massage therapy works best as part of a comprehensive approach to back pain. Here are evidence-based strategies to enhance your results:
Combine with Exercise
Research consistently shows that massage plus exercise outperforms either treatment alone. While massage releases tight muscles and reduces pain, exercise strengthens weak muscles and improves stability. Core strengthening, gentle stretching, and low-impact activities like walking or swimming complement massage therapy well.
Address Postural Factors
If your back pain stems from poor posture—and much of it does—massage provides temporary relief unless you also address the underlying habits. Evaluate your workstation ergonomics, sleeping position, and daily movement patterns. Your massage therapist may offer specific recommendations based on what they observe in your muscle patterns.
Consistency Matters
Sporadic massages help, but consistent treatment works better. For chronic back pain, consider weekly sessions initially, transitioning to bi-weekly and then monthly as your condition improves. This allows tissue changes to accumulate rather than constantly starting over.
Communicate with Your Therapist
Tell your therapist what's working and what isn't. If certain techniques provide relief, mention it. If something increases your pain, speak up. The most effective treatment is collaborative—your feedback helps your therapist refine their approach to your specific needs.
- Be specific about your pain location, type, and triggers
- Report any changes between sessions—better or worse
- Mention activities that help or aggravate your pain
- Ask about self-care techniques to use between sessions
- Discuss your goals and timeline expectations
When Massage May Not Be Enough
While massage therapy helps many people with back pain, it's not a cure-all. Certain conditions require additional or different treatment:
- Herniated discs causing nerve compression may need medical intervention
- Spinal stenosis often requires medical management
- Inflammatory conditions (ankylosing spondylitis, etc.) need appropriate medical treatment
- Fractures or structural instability require medical care first
- Pain from internal organ problems won't respond to massage
- Severe or worsening symptoms warrant medical evaluation
Massage can still play a supportive role alongside medical treatment for many of these conditions, helping manage muscle tension and stress. But it should complement, not replace, appropriate medical care when needed.
Frequently Asked Questions
How often should I get massage for chronic back pain?
Is deep tissue massage or Swedish massage better for back pain?
Can massage make back pain worse?
Should I get massage if I have a herniated disc?
How long do the benefits of massage last for back pain?
Is massage covered by insurance for back pain?
Can I massage my own back for pain relief?
Should I apply heat or ice before/after massage for back pain?
The Bottom Line: Does Massage Work for Back Pain?
The evidence is clear: massage therapy is a legitimate, research-supported treatment for back pain—particularly for nonspecific low back pain, muscle tension-related pain, and chronic conditions where stress plays a role—it's not magic, and it's not appropriate for every type of back pain, but for the right conditions, it offers meaningful relief with minimal risk.
The key is approaching massage as part of a comprehensive strategy. Combined with appropriate exercise, attention to posture and ergonomics, and medical care when needed, massage therapy can be a valuable tool in managing back pain—for many people, it offers something medications can't: lasting relief without side effects, improved body awareness, and a better quality of life.
If you've been wondering whether massage might help your back pain, the research suggests it's worth trying. Start with a qualified therapist, communicate openly about your condition, and give it enough time—usually several sessions—to assess effectiveness. Your back may thank you.